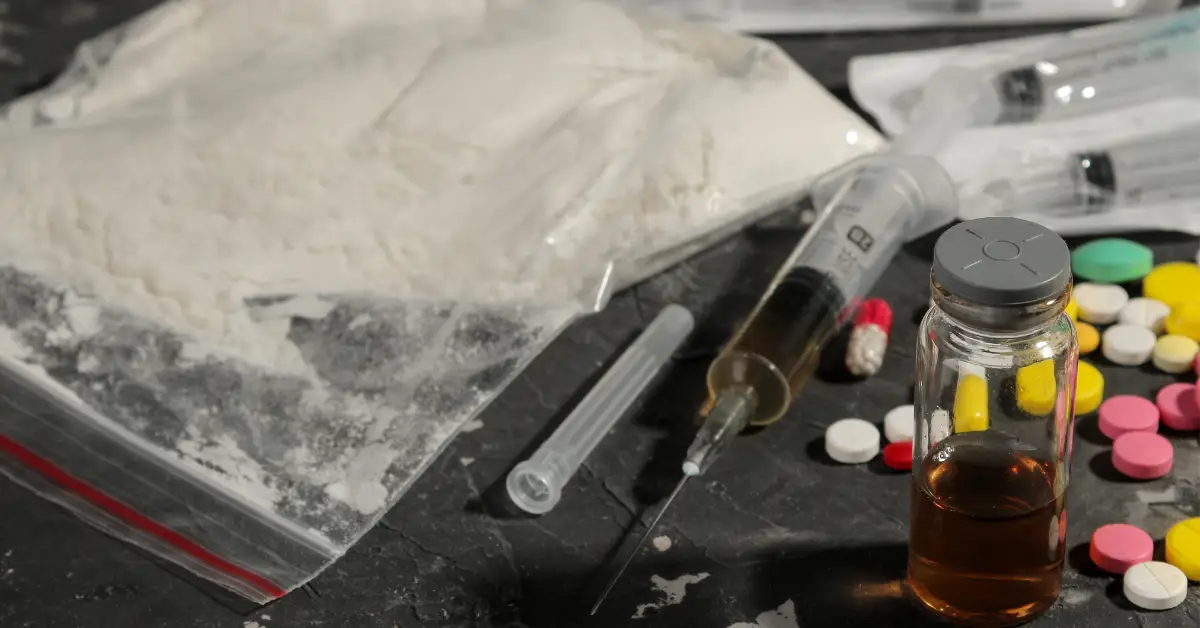
Substance abuse refers to the harmful or hazardous use of psychoactive substances, including alcohol and illicit drugs. It often involves using these substances in a way that is not intended or recommended, leading to negative consequences.
Addiction, or substance use disorder, is a chronic disease characterised by compulsive drug seeking and use despite harmful consequences. It involves physical and psychological dependence on the substance.
Cimas Health Group’s doctor, Sepiso Faith Zulu explained that the most abused substances include alcohol, nicotine, marijuana, opioids, cocaine and benzodiazepines.
“Casual substance use can progress into dependence or addiction through stages. These are experimental use, occasional use, regular use and finally dependence and addiction. Factors such as genetic predisposition, environmental influences and psychological factors can accelerate this progression,” Dr Zulu explained.
‘It should be noted that addiction is considered both a disease and a behavioural disorder. It is a chronic brain disorder that affects behaviour and decision-making, leading to compulsive substance use despite harmful consequences.”
Dr Zulu said the brain’s reward system is heavily involved in addiction. “Substances affect neurotransmitters such as dopamine, which create feelings of pleasure and reinforce the behaviour. Overtime, the brain’s structure and function change, making it difficult to stop using the substance,” she noted.
“Some of the primary causes or triggers of substance abuse include stress, emotional distress, environmental cues, social influences, trauma and peer pressure. These factors can lead individuals to use substances as a coping mechanism.”
Dr Zulu added: “Genetics also play a significant role when it comes to addiction. Studies suggest that genetics can account for 40 to 60% of an individual’s vulnerability to addiction. Specific genes related to dopamine regulation are often implicated.”
She went on to explain that mental health disorders intersect with substance use.
“Mental health disorders and substance use disorders often co-occur. Individuals may use substances to self-medicate symptoms of mental health issues, which can exacerbate both conditions,” Dr Zulu noted.
“Environmental or social factors increase the risk of addiction. These factors include family dynamics, peer pressure, cultural norms, media influence and availability of substances. Stressful environments and lack of support systems also contribute.”
Dr Zulu said adolescents and young adults are particularly vulnerable due to the ongoing development of the brain, especially the prefrontal cortex, which is responsible for decision-making and impulse control.
“Some of the early warning signs that someone may need help include changes in behaviour, neglecting responsibilities, withdrawal from social activities, physical health issues and increased secrecy,” she said.
“The most appropriate treatment for a patient is tailored based on the individual’s specific needs, including the type of substance used, the severity of addiction, co-occurring mental health disorders and personal circumstances.”
Dr Zulu went on to explain the difference between inpatient and outpatient treatment programmes.
“Inpatient treatment involves staying at a facility for a period, providing intensive care and support while outpatient treatment allows individuals to live at home while attending scheduled treatment sessions.”
“Medications can help manage withdrawal symptoms, reduce cravings and
treat co-occurring mental health conditions. Examples include methadone for opioid addiction and naltrexone for alcohol dependence.”
“Relapse is addressed through ongoing support, therapy and sometimes medication adjustments. It is viewed as a part of the recovery process, not a failure,” Dr Zulu added.
She pointed out that recovery timelines vary widely as some individuals may achieve significant progress in a few months, while others may take years.
“Full recovery is possible, but it often requires lifelong management. Family and community support are crucial. They provide emotional support, help maintain accountability and can assist in creating a stable environment for recovery,” Dr Zulu explained.
“Several kinds of therapy or counselling tend to be the most effective. Cognitive-behavioural therapy (CBT), motivational interviewing, dialectical behaviour therapy (DBT) and group therapy are commonly effective.”
She continued: “Support to help patients rebuild their lives, professionally and socially after addiction includes vocational training, job placement services, social skills training and ongoing counselling to help reintegrate into society.”
“Some of the most effective strategies for preventing substance abuse include education, early intervention and strengthening community and family bonds. Prevention education should begin in early childhood and continue through adapting the content to be age appropriate.”
Dr Zulu noted that lifestyle choices or habits that include healthy coping mechanisms can help reduce the risk of addiction.
“Cimas offers a range of services to help people with substance abuse or addiction problems. These include counselling, rehabilitation programmes, support groups and medical treatment for substance abuse and addiction,” she said.